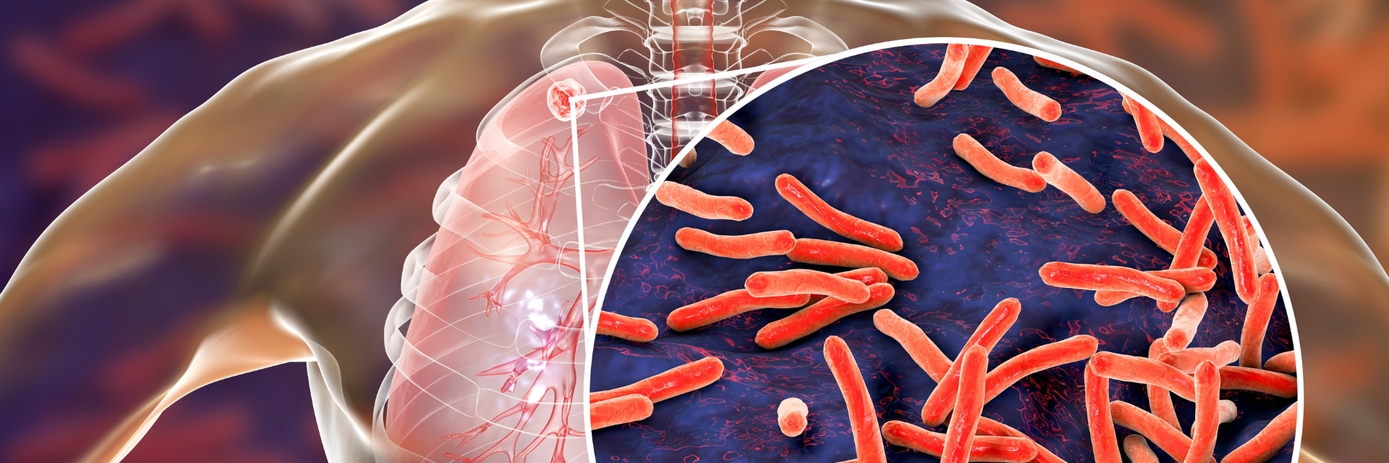
Each year, the 24th of March marks World Tuberculosis Day, an important opportunity to raise awareness and reflect on the global fight against one of humanity’s deadliest infectious diseases: tuberculosis (TB). This date holds historical significance—it marks the moment in 1882 when Dr. Robert Koch announced his groundbreaking discovery of the TB bacillus (Mycobacterium tuberculosis), paving the way for advancements in controlling the disease.
In Dr. Koch’s time, TB was rife across Europe and the Americas, claiming the lives of 1 in every 7 people. Since then, advancements in prevention, diagnosis and antibiotic treatment have significantly reduced the global burden of TB. However, the fight is far from over: TB remains a significant global health challenge, disproportionately impacting vulnerable populations and low-income regions1.
The WHO Global Tuberculosis Report 2024 (covering stats from 2023), provides the latest insights into the global TB landscape, and paints a complex picture of progress and ongoing challenges. It highlights the urgent need for innovation and collaboration to meet the WHO’s End TB Strategy's goal of eliminating 80% of new cases by 2030.
To help raise awareness on this important day, we’re sharing our key takeaways from the report–examining the strides made, the obstacles ahead, and the critical role of diagnostic testing in the global fight against TB.
The big picture
TB continues to be a formidable global health challenge. In 2023, 10.8 million people developed TB, a slight increase from 10.6 million in 2022. TB has reclaimed its position as the world’s leading infectious disease killer, surpassing COVID-19, which held the top spot since 2020. While COVID-19 mortality has declined due to new vaccines, treatments, and global response efforts, TB’s death toll remains disturbingly high.
In 2023, the disease caused 1.25 million deaths worldwide, marking a small decline from 1.32 million in 2022. The return of TB as the leading infectious killer highlights the importance of sustained investment in TB diagnostics, prevention and treatment to match the urgency that drove the COVID-19 response.
Adding to the complexity of controlling TB is the challenge posed by latent tuberculosis infection (LTBI). It is estimated that a staggering one-quarter of the global population are infected with a latent TB infection2, where the infection remains dormant without causing symptoms. For most individuals, this condition remains inactive; however, 5–10% of those with LTBI will develop active TB at some point in their lives3, often triggered by factors such as weakened immunity. Once active and symptomatic, TB can be transmitted to others. It is estimated that people with symptomatic TB can infect up to 15 other people through close contact over the course of a year. This latent reservoir is a silent driver of the epidemic, continuously feeding the pool of active TB cases. Tackling LTBI, particularly in high-risk groups such as the immunosuppressed, is critical for breaking the cycle of transmission.
The impact on high-burden populations
In 2023, 50% of TB-affected households faced catastrophic costs, defined as expenses exceeding 20% of their annual income for diagnosis, treatment and prevention. These costs can plunge families deeper into poverty, perpetuating the cycle of illness and financial hardship. The financial burden of TB reinforces its status as a "disease of deprivation," disproportionately affecting those in low-income settings with limited access to healthcare and social support.
TB remains a leading cause of death among people living with HIV, with 161,000 TB-related deaths recorded in this group in 2023. This stark figure highlights the dangerous correlation between HIV and TB, as people with compromised immune systems are more likely to progress from LTBI to active disease. Despite this high risk, TB testing in HIV-positive individuals often presents challenges due to low white blood cell counts, which can reduce the reliability of traditional diagnostic methods.
Sensitive diagnostic tools like Revvity’s Interferon Gamma Release Assay, the T-SPOT.TB test are invaluable in identifying a potential LTBI in these vulnerable populations. By standardising the number of white blood cells analysed, the T-SPOT.TB test ensures accurate results, even in those with weakened immune systems4,5.
Closing the diagnostic gap
Access to robust diagnostics is a critical pillar of effective TB control. While diagnostic rates are improving, with 8.2 million cases newly diagnosed (up from 7.5 million in 2022), the disease continues to evade detection in many. An estimated 2.7 million cases remain undiagnosed or unreported, leaving significant gaps in treatment and prevention.
This diagnostic gap is an imperative issue to address if we are to meet the targets set out by the WHO’s End TB Strategy. Undetected cases not only leave individuals vulnerable to severe health complications but also allow TB to spread further within communities, perpetuating its global burden. In 2023, 48% of newly diagnosed TB cases were tested using WHO-recommended rapid diagnostic tools, reflecting significant progress. However, this figure still falls far short of the WHO's ambitious target of 100% diagnostic coverage by 2027.
Improving TB diagnostics isn't just about increasing coverage; it's about deploying tools that are scalable, reliable and able to meet the needs of diverse populations. Achieving 100% rapid diagnostic coverage by 2027 will require robust diagnostic solutions like the T-SPOT.TB test, along with better awareness, increased investment and global collaboration.
A pathway to better prevention
Prevention is one of the most powerful tools in the fight against tuberculosis, yet the recent data shows substantial shortfalls in preventive treatment coverage. For example, in 2023, only 21% of household contacts of TB patients—individuals who are frequently exposed to the disease—received preventive treatment. This leaves millions at risk of developing active TB, creating a reservoir of future cases that perpetuates the epidemic.
Thankfully, progress is better among people living with HIV, a group at much higher risk of reactivating LTBI due to compromised immune systems. In 2023, 56% of HIV-positive individuals received preventive treatment, a more encouraging figure but still far below WHO targets. Ensuring preventive care for these high-risk populations is a crucial step toward breaking the cycle of TB transmission at its source.
Preventive treatment typically involves antibiotic regimen with isoniazid and rifapentine or rifampicin, which have proven highly effective in reducing the risk of progression to active TB6. However, barriers such as limited access to healthcare, financial constraints and a lack of awareness about the importance of LTBI testing continue to hinder progress.
The promise of new TB vaccines offers renewed hope in the fight against the disease. Currently, there are six vaccines in Phase III trials, with plans for rollout by 2028. These vaccines could transform TB prevention, particularly in regions with high burdens of the disease. Unlike the traditional BCG vaccine, which provides limited protection and is primarily effective in young children, these new vaccines aim to offer broader, more robust immunity across all age groups.
Taking the fight to TB
TB is once again the world’s deadliest infectious disease, but the path to its elimination is clear: better diagnostics, stronger prevention and global collaboration. A critical aspect of this fight lies in addressing latent infections, a critical and silent driver of the disease. Tools like T-SPOT.TB are already making a vital difference by accurately detecting LTBI, particularly in high-risk populations where traditional tests often fall short.
This World Tuberculosis Day, let’s commit to amplifying awareness, driving innovation, and working together to achieve the End TB Strategy’s goals. With sustained effort, we can continue to turn the tide on TB and work towards a healthier, TB-free future for all.
References
- Global tuberculosis report 2024. Geneva: World Health Organization; 2024. Licence: CC BY-NC-SA 3.0 IGO.
- Ding, C. et al. Prevalence trends of latent tuberculosis infection at the global, regional, and country levels from 1990–2019. International Journal of Infectious Diseases 122, 46–62 (2022).
- Kiazyk, S. & Ball, T. B. Latent tuberculosis infection: An overview. Canada Communicable Disease Report 43, 62 (2017).
- Oxford Immunotec T-SPOT.TB Package Insert PI-TB-IVD-UK-v5. Abingdon, UK. November 2023.
- World Health Organization. WHO operational handbook on tuberculosis. October 1, 2022.
- Huaman, M. A. & Sterling, T. R. Treatment of latent tuberculosis infection – An Update. Clin Chest Med 40, 839 (2019).
Rewity, Inc. does not endorse or make recommendations with respect to research, medication, or treatments. All information presented is for informational purposes only and is not intended as medical advice.