Background
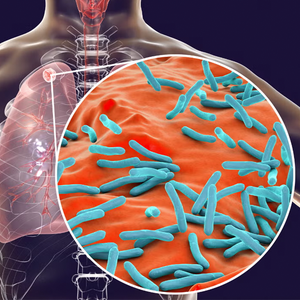
Pre-eclampsia is a complication of pregnancy marked by high blood pressure and presence of protein in the urine (proteinuria). Pre-eclampsia affects 2–8% of pregnancies. The incidence is increasing with the global increase in maternal age, obesity and the use of assisted reproductive techniques. It also follows the rising incidence of diabetes, hypertension, and renal disease – all are known co-morbidities that predispose sufferers to pre-eclampsia during pregnancy. Pre-eclampsia develops as a result of abnormal blood flow to and within the placenta, which in turn can cause growth-restriction or preterm birth of the child. When left untreated, pre-eclampsia can lead to eclampsia, a serious condition that can endanger the mother’s life. [1]
In one third of the cases the condition leads to delivery at <37 weeks’ gestation (preterm pre-eclampsia) and in two thirds delivery occurs at ≥37 weeks (term pre-eclampsia). [2,3] There is evidence that pre-eclampsia also leads to long term health problems. Women who develop pre-eclampsia have twice the risk of cardiovascular disease (CVD) at some stage in their life.
It is not known whether pre-eclampsia causes vascular damage that ultimately leads to CVD or whether women prone to CVD are stressed by pregnancy to develop pre-eclampsia.[5,6] Children born to pre-eclamptic mothers have twice the risk of cerebral palsy; this increased risk being mediated through premature birth, growth-restriction or both. Offspring exposed to pre-eclampsia also have higher blood pressure and body mass index, compared to those born after normal pregnancy, and have increased risk of CVD and diabetes in adult life.[5,6]
Clinical Diagnosis
While the direct cause of pre-eclampsia is unknown, researchers agree that if symptoms such as high blood pressure and proteinuria occur from week 20 onwards until 6 weeks after delivery, there is a high risk that the placenta will be adversely affected. [8] In the absence of proteinuria, the finding of maternal organ dysfunction is sufficient to make the diagnosis of pre-eclampsia.
Testing
PlGF and sFlt-1 are found to be key factors in the pathophysiology of pre-eclampsia. [9] In pregnancies that develop pre-eclampsia, maternal serum placental growth factor (PlGF) levels decrease significantly, while soluble fms-like tyrosine kinase 1 (sFlt-1) levels increase several weeks prior to clinical symptom onset. [9]
Thus, PlGF and sFlt-1 are important biomarkers used to identify high risk women that are likely to develop preterm pre-eclampsia later in their pregnancy and to predict the onset of pre-eclampsia. Biomarker levels are also found to be correlating with severity of disease. [9]
A combined screening program for pre-eclampsia is recommended by international guidelines.[7, 8] to identify women at high risk of pre-eclampsia in the early stages of pregnancy. The combined screening program consists of the PlGF blood test, maternal medical history assessment, mean arterial blood pressure measurement and, if available, uterine artery Doppler ultrasonography. The risk is calculated with a software using a risk calculation algorithm (e.g. LifeCycle).
Treatment
Aspirin treatment is highly effective in the prevention of early and preterm pre-eclampsia.[4, 5] The timeframe for pre-eclampsia screening is the first trimester, when low-dose aspirin therapy shows the best results in the prevention of pre-eclampsia. To achieve maximum effectiveness, aspirin therapy should be started before 16 weeks of gestation among women at high risk of pre-eclampsia.[7]
Inheritance
Certain maternal characteristics and factors are known to increase the risk of pre-eclampsia, such as patient’s personal and family history. Other factors increasing the risk are:
- Advanced maternal age
- BMI (Body Mass Index) greater than 35
- Afro-Caribbean and South Asian racial origin
- Chronic hypertension
- Diabetes mellitus
Systemic lupus erythematosus - Antiphospholipid syndrome
- Conception by in vitro fertilization
References:
- Tranquilli AL, et al., The classification, diagnosis and management of the hypertensive disorders of pregnancy: A revised statement from the ISSHP. Pregnancy Hypertens 2014; 4: 97-104.
- Verghese L, et al., Antenatal screening for pre-eclampsia: evaluation of the NICE and pre-eclampsia community guidelines. J Obstet Gynaecol. 2012;32(2):128–131
- World Health Organization. Make Every Mother and Child Count. World Health Report, 2005. Geneva, Switzerland: World Health Organization; 2005.
- Kuklina EV, et al. Hypertensive disorders and severe obstetric morbidity in the United States. Obstet Gynecol 2009; 113:1299-306
- Wu P et al., Preeclampsia and Future Cardiovascular Health: A Systematic Review and Meta-Analysis. Circ Cardiovasc Qual Outcomes 2017;
- Veerbeek JH et al., Cardiovascular disease risk factors after early-onset preeclampsia, late-onset preeclampsia, and pregnancy-induced hypertension. Hypertension 2015; 65: 600-606.
- Bujold E, et al.. Prevention of preeclampsia and intrauterine growth restriction with aspirin started in early pregnancy: a meta-analysis. Obstet Gynecol. 2010 Aug;116
- Poon L, et al. The International Federation of Gynecology and Obstetrics (FIGO) Initiative on Pre-eclampsia: A Pragmatic Guide for First-Trimester Screening and Prevention. International Journal of Gynegology & Obstetrics. May 2019
- Lecarpentier E1, Tsatsaris V. Angiogenic balance (sFlt-1/PlGF) and preeclampsia. Ann Endocrinol (Paris). 2016 Jun;77(2):97-100.
Instruments for pre-eclampsia screening & management